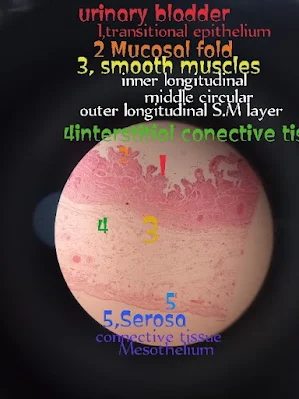
Under The Light Microscopic View
1. Transitional Epithelium:
2. Mucosal Folds:
3. Smooth Muscle Layers (Detrusor Muscle):
- Inner Longitudinal Layer
- Middle Circular Layer
- Outer Longitudinal Layer
4. Interstitial Connective Tissue:
5. Serosa:
Identifying histological features on urinary bladder slides involves examining the tissue under a microscope. Here are some key points to look for when identifying structures in urinary bladder histology slides:
1.Urothelium (Transitional Epithelium):
Typically stratified and can have umbrella cells at the apical surface.
Appearance changes with distension: when the bladder is empty, cells are more rounded, and when the bladder is full, cells flatten out.
The innermost layer lining the urinary bladder.
2.Lamina Propria:
Connective tissue layer beneath the urothelium.
Contains blood vessels, nerves, and scattered fibroblasts.
3.Muscularis Layer:
Smooth muscle layer responsible for bladder contraction.
Composed of inner longitudinal and outer circular smooth muscle fibers.
4.Adventitia/Serosa:
Outermost connective tissue layer (adventitia) or serosa (if covered by peritoneum).
5.Blood Vessels:
Look for blood vessels within the lamina propria and adventitia/serosa.
6.Nerves:
Fine nerve fibers may be visible, especially in the lamina propria.
7.Blood Supply and Lymphatics:
Identify blood vessels and lymphatic vessels within the tissue.
8.Goblet Cells:
In some areas, you may find goblet cells in the urothelium, particularly in the region near the urethra.
9.Inflammatory Cells:
Look for signs of inflammation, such as infiltrating immune cells, which may indicate a pathological condition.
10.Connective Tissue Fibers:
Collagen and elastic fibers may be present in the lamina propria.
Students can use these key features for examination purpose:
Transitional Epithelium:
- The slide showcases the bladder’s characteristic lining, which is composed of a specialized epithelium that can stretch and contract. This layer is crucial for allowing the bladder to accommodate varying volumes of urine.
- Beneath the epithelial layer lies the thick lamina propria, a dense connective tissue layer that provides structural support and houses blood vessels and nerves.
- The histology slide includes a section of the bladder wall, but does not show the lumen, the internal cavity where urine is stored.
- A striking feature of the slide is the muscularis layer, which is notably thick and composed of three distinct layers of smooth muscle. These layers work in harmony to facilitate the contraction of the bladder during urination.
- The slide lacks glandular structures and there is no distinct submucosal layer, which is typical of bladder histology, highlighting the organ's specialized function in storing and expelling urine.
Urnairy Bladder Image Under the Light Microscopic
Here is a description of the key areas:
Transitional Epithelium (Urothelium): This is the innermost layer lining the bladder lumen. It appears as multiple layers of cells, which are more cuboidal in the deeper layers and become more flattened towards the surface. This layer is designed to stretch as the bladder fills with urine.
Lamina Propria: Situated beneath the transitional epithelium, this layer consists of loose connective tissue containing blood vessels and nerves. It supports the epithelium and provides a flexible base for the bladder’s stretching capacity.
Muscularis Propria (Detrusor Muscle): This layer is made up of smooth muscle fibers arranged in three layers (inner longitudinal, middle circular, and outer longitudinal). The muscle fibers are responsible for the contraction of the bladder during urination.
Adventitia/Serosa: The outermost layer of the bladder, composed of connective tissue, which may either be the adventitia (when the bladder is located retroperitoneally) or serosa (when it is covered by peritoneum). This layer protects and anchors the bladder in place.
Each of these layers plays a crucial role in the bladder’s function of storing and expelling urine. The transitional epithelium allows for stretching, the lamina propria provides structural support, the detrusor muscle facilitates contraction, and the adventitia/serosa provides external protection and support.
Gross Anatomy of the Urinary Bladder
The urinary bladder is a hollow, muscular organ located in the pelvis, just behind the pubic symphysis. It serves as a temporary reservoir for urine. The bladder's shape and size vary depending on the amount of urine it contains. When empty, it resembles a deflated balloon and is somewhat pyramidal in shape. The bladder has four main parts: the apex (which points towards the abdominal wall), the body (the main part), the fundus (the base or posterior surface), and the neck (which leads into the urethra). The bladder walls are lined with a mucous membrane, and its capacity can range from 400 to 600 ml in adults, although it can hold more if necessary.
Physiology of the Urinary Bladder
The primary function of the urinary bladder is to store urine until it is excreted from the body. Urine enters the bladder via the ureters from the kidneys and exits through the urethra. The bladder is lined with transitional epithelium, which allows it to stretch as it fills. The detrusor muscle, a layer of smooth muscle, contracts during urination to expel urine. The process of urination (micturition) is controlled by both involuntary and voluntary mechanisms. Stretch receptors in the bladder wall signal the brain when the bladder is full, triggering the urge to urinate. The internal urethral sphincter, controlled involuntarily, relaxes, and the external urethral sphincter, which is under voluntary control, must be consciously relaxed to allow urination.
Histopathology of the Urinary Bladder
Histopathology involves examining tissues from the urinary bladder under a microscope to identify diseases. The bladder's transitional epithelium is unique and can undergo changes in response to different pathological conditions. For instance, chronic irritation, such as from recurrent infections or bladder stones, can cause metaplasia, where the normal bladder lining transforms into a different type of epithelium. Inflammation of the bladder, known as cystitis, often presents with an increase in inflammatory cells within the bladder wall. In more severe conditions, such as bladder cancer, abnormal cells may be observed infiltrating the bladder's layers, indicating malignancy. Bladder cancer often originates in the transitional epithelium and can spread into the deeper layers of the bladder wall.
Clinical Significance of the Urinary Bladder
The urinary bladder is central to various medical conditions that can significantly affect a person’s quality of life. Urinary tract infections (UTIs) are common and can involve the bladder, leading to cystitis, characterized by symptoms such as burning during urination, increased frequency, and urgency. Bladder stones can form from crystallized minerals, leading to pain, infection, or blockage of urine flow. Incontinence, the inability to control urination, can occur due to issues with the bladder or sphincters, often seen in older adults or after childbirth in women. Bladder cancer is another critical condition, particularly prevalent among smokers, and typically presents with painless hematuria (blood in the urine). The early detection and treatment of bladder-related conditions are crucial for preventing complications, ensuring proper urinary function, and maintaining overall health.

















0 Comments